The holidays are often portrayed as cozy, warm, and full of connection — twinkling lights, family dinners, shared laughter.
But for many people living with post-traumatic stress or carrying the weight of a difficult past, this season feels very different.
You may show up with a smile, bring food, help set the table, chat with relatives…
But inside, your body feels tight.
Your chest feels heavy.
Your mind is alert, even when nothing is actually wrong.
If you’ve ever wondered why the holidays feel more draining than comforting, you’re not alone.
Many people in Vancouver, Burnaby, and New Westminster experience a rise in PTSD symptoms at this time of year — and most never say it out loud.
This isn’t about forcing holiday cheer.
It’s about understanding why your nervous system reacts the way it does, and how trauma-informed therapy can help you move through this season with more softness and safety.
Why Holidays Trigger Trauma: The Body Remembers What the Mind Tries to Forget
Trauma doesn’t always show up as memories.
More often, it shows up as sensations — a clenched jaw, a knot in the stomach, a sense of dread, or an urge to leave the room without knowing why.
During the holidays, people commonly feel:
- on edge
- overstimulated
- emotionally distant
- easily triggered
- overwhelmed by noise or expectations
This isn’t because you’re “too sensitive.”
It’s because trauma lives in the nervous system — and the holidays tend to recreate the very conditions that once felt unsafe.
Common Trauma Triggers That Resurface During the Holidays
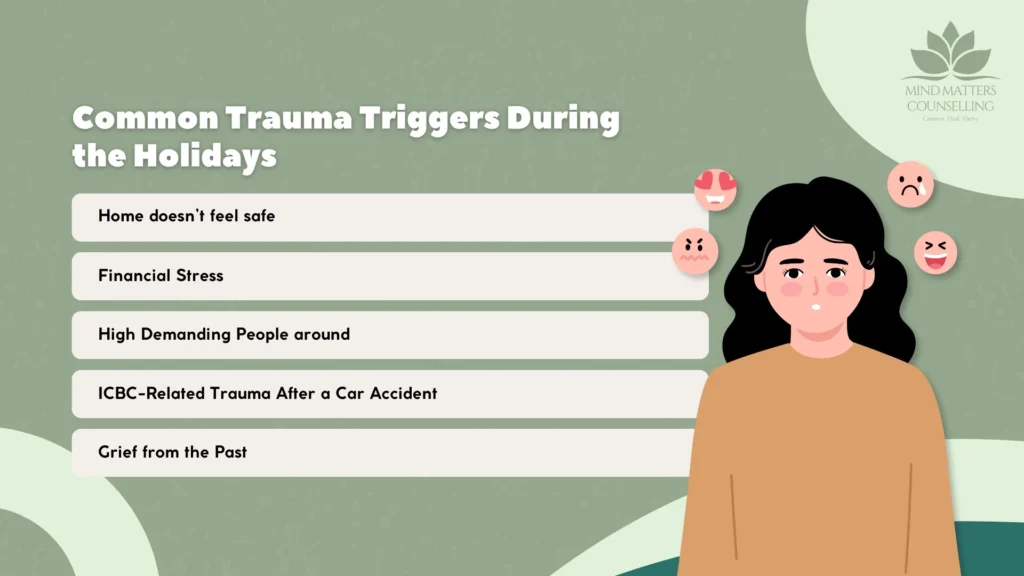
1. Returning to Environments Where Pain Once Lived
Going “home” can pull you backward emotionally, even if your adult life is stable.
The nervous system responds to familiarity, not logic.
2. Family Dynamics That Echo Old Wounds
Holidays can bring back feelings of:
- being criticized
- needing to stay small
- conflict or unpredictability
- emotional neglect
- pressure to keep the peace
Old roles return before you even notice it happening.
3. Sensory Overload
Crowded gatherings, noise, lights, travel, and busy schedules make regulation harder.
Your system gets overwhelmed faster.
4. ICBC-Related Trauma After a Car Accident
Clients recovering from motor vehicle accidents often experience a spike in anxiety and PTSD symptoms around:
- winter driving
- early sunsets
- heavy traffic
- holiday travel
An ICBC counsellor can help make sense of this — your body might feel unsafe even when you are physically safe.
5. Grief, Loss, and Emotional Distance
The holidays can highlight:
- missing loved ones
- estranged relationships
- unmet childhood needs
- feeling outside the family system
For many, this is the quiet part of the season no one talks about.
How PTSD Shows Up During Holiday Gatherings
Trauma responses aren’t always dramatic.
Most are invisible and internal.
People often describe:
- hypervigilance
- jumpiness
- numbness or zoning out
- irritability after too much stimulation
- heaviness in the chest
- emotional flashbacks
- exhaustion after social events
These reactions aren’t weakness.
They are survival responses your body learned during hard times.
Understanding What’s Happening: A Nervous System Perspective
Your body doesn’t track dates — it tracks signals of danger or safety.
Holiday gatherings can activate old patterns without your permission.
You may find yourself in:
Fight – irritability, defensiveness
Flight – wanting to leave early, staying busy
Freeze – shutting down, feeling detached
Fawn – people-pleasing, over-helping, avoiding conflict
These are not personality traits.
They are trauma patterns your body learned to stay alive.
How Trauma Therapy Supports You Through the Holidays
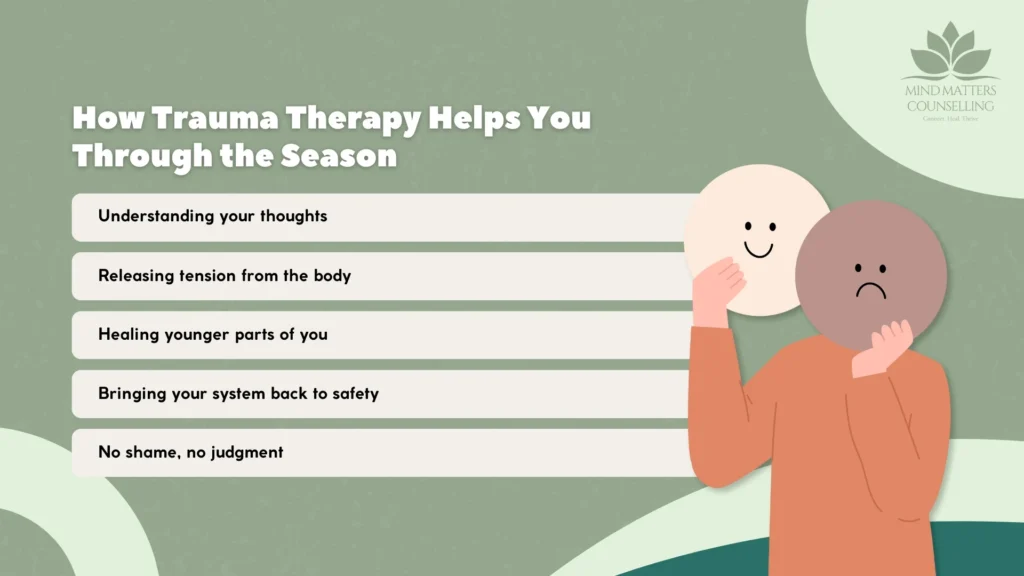
You don’t have to avoid the holidays, and you don’t have to push yourself through them either.
Therapy gives you tools, language, and support to understand what your body is trying to protect you from.
At Mind Matters Counselling, therapists across Vancouver, New Westminster, and Burnaby use approaches such as:
• Trauma-Focused CBT (TF-CBT)
Helps you understand how trauma shaped certain thoughts, fears, and interpretations.
• Somatic Therapy
Supports you in noticing where trauma sits in the body and how to gently regulate it.
• Internal Family Systems (IFS)
Explores younger, protective parts of you — the ones who learned to stay quiet, perfect, or hyper-alert.
• Grounding & Nervous System Regulation
Teaches your body how to shift out of fight-or-flight into a state of safety.
• Psychoeducation with Compassion
Helps you understand your patterns without shame or self-blame.
Therapy isn’t about “getting over” trauma.
It’s about creating safety inside yourself, slowly and with gentleness.
If This Season Feels Heavy, You’re Not Alone
Many people appear high-functioning but feel triggered and overwhelmed underneath.
Your feelings make sense.
Your body is trying to protect you — even if the danger is no longer here.
You don’t have to navigate this alone.
If you’re noticing trauma or PTSD symptoms this season — whether from childhood trauma, relationship trauma, or an ICBC-related accident — therapy can help you feel grounded again.
Book a session with a trauma therapist at Mind Matters Counselling today.
FAQs
- 1. What are the 5 symptoms of PTSD?People with Post-Traumatic Stress Disorder may experience a combination of symptoms, commonly grouped into five areas:
- Intrusive memories (flashbacks, nightmares, distressing thoughts)
- Avoidance of reminders related to the trauma
- Negative changes in thoughts and mood (fear, guilt, detachment, low mood)
- Changes in physical and emotional reactions (hypervigilance, irritability, sleep issues)
- Emotional numbing or feeling disconnected from oneself or others
- 2. What is the best therapy for PTSD?There is no “one-size-fits-all,” but the most effective, evidence-based therapies for PTSD include:
- Trauma-Focused CBT (TF-CBT)
- EMDR (Eye Movement Desensitization and Reprocessing)
- Somatic or body-based trauma therapy
- Trauma-informed counselling
- 3. What does a PTSD episode look like?A PTSD episode can feel like the trauma is happening all over again. Common signs include:
- Intense panic or fear
- Flashbacks or intrusive memories
- Physical symptoms like a racing heart, sweating, shaking
- Dissociation (feeling “not present” or disconnected from reality)
- Emotional overwhelm or shutting down
- 4. Will I ever be normal after PTSD?Yes—healing from PTSD is absolutely possible. With the right therapy and support, many people regain a sense of safety, connection, and control. “Normal” may look different from before the trauma, but clients often reach a place where their symptoms no longer dominate their lives.
- 5. How do I get out of a PTSD episode?Grounding techniques can help bring you back to the present moment, such as:
- Slow, deep breathing
- Naming objects around you (5-4-3-2-1 grounding)
- Touching something with texture (ice, fabric, etc.)
- Noticing your feet on the ground
- Repeating calming statements like “I am safe right now”
- 6. What helps PTSD the most?The most effective support for PTSD typically includes:
- Professional trauma therapy (EMDR, CBT, somatic therapies)
- Consistent emotional support from trusted people
- Healthy coping tools such as grounding, mindfulness, and breathwork
- Regular routines, sleep hygiene, and physical self-care
- 7. Is PTSD a mental illness?Yes, PTSD is classified as a mental health condition that can develop after experiencing or witnessing a traumatic event. It is not a sign of weakness—it's a normal response of the brain and body trying to cope with something overwhelming.
- 8. What is the fastest way to calm PTSD?The quickest short-term strategies include:
- Deep, slow breathing (activates the body’s calming system)
- Grounding techniques to reorient to the present
- Cold stimulation (splashing cold water, holding an ice cube)
- Safe movement like pacing, stretching, or shaking out tension